In this article you will learn:
What is progesterone?
What is Oestradiol?
What is the difference between perimenopause and menopause?
What symptoms can be expected during perimenopause?
What does oestrogen do during perimenopause?
What does progesterone do during perimenopause?
What are some signs of low progesterone?
What are some signs of high oestradiol?
What are some signs of low oestradiol?
What are some symptoms or causes of low progesterone and/or high/low oestradiol?
What can blood tests and functional tests help with during perimenopause?
Premature menopause – what is it?
Is it perimenopause, thyroid issues or both?
Partial hysterectomy (surgical removal of your uterus but not ovaries)
Mirena® – what does it do?
READ THE FULL ARTICLE BELOW | ||
|---|---|---|
AUTHOR: Shona Mackenzie (Naturopath & Medical Herbalist) |
Your Main Hormones Explained
1. What Is Progesterone?
Progesterone is your main hormone for your cycle health. It is part of a group of steroid hormones called ‘progestogens’. It’s most important role is to hold and sustain the early stages of pregnancy. Progesterone is your calming hormone.
Progesterone is also produced in smaller amounts by the ovaries, adrenal glands and the placenta during pregnancy.
It’s most major production site is by the corpus luteum in the ovaries – a hormone-secreting structure that is formed in the ovaries by a follicle that has matured and released its egg during ovulation. It secretes progesterone and some oestradiol (E2), with the objective to prepare the body for pregnancy if a released egg was fertilised. If not, the corpus luteum breaks down after 10-14 days (during the ‘Luteal Phase’ of a cycle (after ovulation)), and progesterone declines with a new menstrual cycle beginning.
Synthetic hormones found in hormonal birth control are called ‘progestins’, and these prevent ovulation and also thicken cervical mucus (wet eggy white discharge seen pre-ovulation) so sperm fertilisation is ineffective.
Low levels of progesterone can indicate the ovary has failed to release an egg during ovulation. Note: this can occur in polycystic ovary syndrome.
2. What Is Oestradiol?
Oestradiol (E2) or 17-beta oestradiol is the main steroid hormone of three oestrogens (oestrone (E1), oestradiol (E2) and Oestriol (E3)) and it predominantly works to mature and support the female reproductive system.
What to remember about oestradiol:
It is largely made by the ovaries.
It is a steroid hormone and made mostly from cholesterol, but also by fat tissue, the brain, and the walls of blood vessels.
Levels vary during a monthly menstrual cycle.
During your Follicular Phase of your cycle (start of your period to ovulation), oestradiol is increasing from its lowest level to its highest level which is at ovulation.
An increase in oestradiol helps to increase luteinising hormone (LH) levels which aids in maturation of an egg and its release from the ovary (ovulation).
It thickens the lining of the uterus for implantation of a fertilised egg.
It assists development of breast tissue.
It reduces slowly with age, with a major decrease seen at menopause when the ovaries ‘switch off’.
The corpus luteum (see ‘What is Progesterone?’) produces oestradiol in early pregnancy, and then the placenta produces it later.
It strengthens bone and cartilage density.
Men make oestradiol for the production of sperm, through converting testosterone.
Perimenopause – Symptoms, Hormones & Tests
3. What Is The Difference Between Peri-Menopause And Menopause?
Perimenopause and menopause are quite different, though many times they are referred to as one and the same.
Perimenopause can occur 2-12 years before menopause and is the most common time to experience symptoms. Oestrogen during perimenopause can be quite high, where during menopause it is a time of low-oestrogen.
Menopause is the chapter of life that starts one year after your last period, and it is a time when many symptoms will resolve and you can anticipate feeling healthy.
4. What Symptoms Can Be Expected During Perimenopause?
Symptoms that can begin in your 30’s-40s relating to perimenopause are:
Heavier and/or longer periods
Stronger menstrual cramps
Shorter cycles overall (less than 25 days)
Sore, swollen or lumpy breasts
Disturbed sleep
Night sweats, particularly pre-period
New or increased migraine headaches
Fluctuating moods
Weight gain without dietary or exercise changes
If 3 out of the above 9 are experienced by a mid-life woman, then she is likely to be in perimenopause, regardless of regular period cycles. These symptoms can be life-changing and come on quite quickly.
As woman seek help to understand their health, the current course of action can be the pill, oestrogen (HRT), or an antidepressant. Additional oestrogen at a time when oestrogen is already increasing is counter-productive.
5. What Does Oestrogen Do During Perimenopause?
As menopause is a state of low oestrogen and progesterone, and a woman’s reproductive years have ceased, oestrogen has declined. However during perimenopause as it is declining ‘overall’ it is doing so in a wildly fluctuating manner with every cycle. For 20% of women, it can soar highly and then crash to almost nothing again and again. Many women will only experience mild changes.
Symptoms of high oestrogen include:
Breast pain
Heavy periods
Fluid retention
Irritable mood
Symptoms of declining low oestrogen include:
Night sweats
Hot flashes
Heart palpitations
Depression
6. What Does Progesterone Do During Perimenopause?
Progesterone quietly declines during perimenopause and along with it, its soothing influence on the nervous system to support against oestrogen’s roller coaster ride of events. As the ovarian follicles are no longer as active or responsive during your 40s (due to the natural genetic process), progesterone is even harder to make than in your 20s-30s.
7. What Are Some Signs Of Low Progesterone?
Anxiety
Infertility
Insomnia
Irritability
Menorrhagia
PMS/PMDD (Premenstrual dysphoric disorder)
8. What Are Some Signs Of High Oestradiol?
Acne
Dysmenorrhea (painful periods)
Menorrhagia (menstrual bleeding lasting longer than 7 days)
Mood issues
Swelling
Tender breasts
Weight gain
9. What Are Some Signs Of Low Oestradiol?
Bone loss
Hot flashes
Insomnia
Joint pain / skin issues
Low sex drive
Mood issues
Brain fog
Night sweats
Vaginal dryness
Weight gain
10. What Are Some Symptoms Or Causes Of Low Progesterone And/Or High/Low Oestradiol?
High oestradiol:
Existing weight gain/obesity
Diabetes
PCOS
Poor liver function
Gut dysbiosis
Environmental oestrogens (Xenoestrogens)
Alcohol
Inflammation
Ovarian cysts
Peri-menopause (surges of oestradiol)
Low progesterone:
Poor follicle development or quality of the corpus luteum
Painkiller use (can suppress ovulation)
Mirena, IUD/coil can suppress ovulation
Low oestradiol & progesterone:
Sample collection on the wrong day of a cycle
Age (peri-menopause & menopause)
Hysterectomy (with ovaries removed)
Irregular/skipped cycles or anovulation (no ovulation occurring)
Anorexia or underbody weight
Extreme exercise / stress
Hypopituitarism (pituitary gland not communicating)
Hypogonadism (ovaries fail)
Decreased blood flow to the ovaries (e.g. surgery or smoking)
Breastfeeding
Hypothyroidism (underactive thyroid)
PCOS (Polycystic Ovary Syndrome)
Fertility medications
Opioid pain medications (within last 6 months)
Hormonal birth control (pill, ring, patch, implant, injection)
Elevated prolactin
11. What Can Blood Tests And Functional Tests Help With During Perimenopause?
As you enter into perimenopause a naturopath can order a specific range of blood tests and/or functional tests i.e. D.U.T.C.H. tests, to assess what stage your hormones are at. These are vital in providing answers to support your journey. Click here to learn about D.U.T.C.H. tests.
Other Factors To Consider
12. Premature Menopause – What Is It?
Premature menopause, (also known as premature ovarian failure or primary ovarian insufficiency), is explained as the loss of ovarian function before age 40. Factors relating to premature menopause can be genetics, autoimmune disease, and endometriosis.
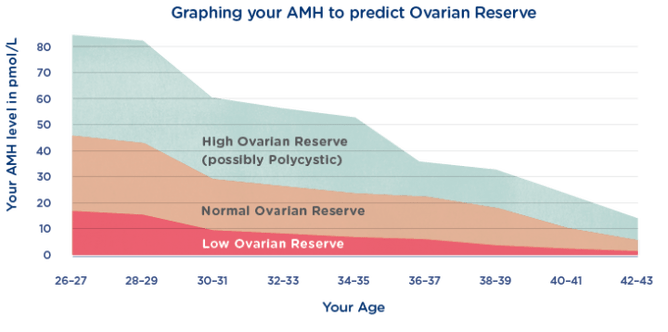
A blood test that can help recognise this specifically is FSH (follicle stimulating hormone), and an Anti-Mullerian Hormone (AMH test) can be of help also.
FSH stimulates the growth of follicles in the ovary before the release of an egg from a follicle during ovulation. It also supports oestradiol production from the ovaries.
If there is a lack of FSH in a women, this can relate to poor ovarian function, as the ovarian follicles do not grow properly, and do not release an egg (a complication related to infertility).
The AMH test represents a women’s egg count, however it does not predict your fertility.
High AMH levels = more eggs and a higher ovarian reserve
Low AMH levels = fewer eggs and a lower ovarian reserve
Graphing your AMH to predict Ovarian Reserve (Repromed.co.nz)
13. Is It Perimenopause, Thyroid Issues Or Both?
Thyroid dysfunction can look a lot like perimenopause as both conditions can cause symptoms of:
Insomnia
Depression
Weight gain
Heavy period
Irregular periods
Hot flashes
Difficulty concentrating/brain fog
Supporting progesterone levels naturally can be very beneficial for good thyroid health.
Conventional Methods For Heavy Periods During Perimenopause
14. Partial Hysterectomy (surgical removal of your uterus but not ovaries)
A hysterectomy is a standard medical treatment approach for heavier periods (and possible pain). It can be necessary for some hormonal cases, but it is highly recommended to review all areas of your health holistically prior to this decision, as the removal of your uterus (only) will not alter your hormones or cause menopause. The underlying cause of why heavy periods and pain were occurring can still exist regardless of no uterus, and so a ‘natural period repair’ approach where oestradiol and progesterone are still supported is important e.g. progesterone to support mood, bones, brain and thyroid health.
NOTE: The natural treatment of heavy periods is beneficial only as a prevention, not as acute support. Lifestyle, diet and correct supplementation can play a large role in prevention, so it is highly recommended that you and a naturopath monitor and treat your cycle BEFORE this becomes a daily complication.
Research studies of women with a hysterectomy have shown:
Long-term risk of vaginal prolapse
Urinary incontinence
Adversely affect your sexual response and ability to orgasm (especially if your ovaries have been removed too)
15. Mirena® – What Does It Do?
A Mirena® is a intrauterine device (IUD) that releases progestin levonorgestrel (a small amount) into the uterus. It works by thinning the uterine lining and decreasing cervical mucus, and it can inadvertently suppress ovulation (but not as often as other progestin-only methods).
A Mirena® inhibits a bleed but allows ovulation and hormones. It is medically recommended during perimenopause for period issues, when high oestrogen levels cause flooding, endometriosis and adenomyosis (cells that grow and proliferate on the inside of the uterus).
Symptoms of the hormonal IUD has been associated with:
Depression
Inability to cope with stress
Points To Remember During Your Perimenopause Journey
Your period will become irregular i.e. start and stop.
Regular blood tests can be a great support to monitor hormonal levels during this time which your naturopath can help interpret and guide you on.
Preventative monitoring and rebalancing of your hormones can support a healthy transition through perimenopause.
Diet and lifestyle can play an important role in hormonal health.
Perimenopause is a perfectly natural process that when you learn and understand the normal symptoms, this will in turn help you to feel normal and not a crazy woman. (Pamela Boggs)
How Can You Help Your Transition During Perimenopause?
As recommended by Lara Briden (Period Repair Manual):
Support progesterone
Metabolise oestrogen
Reduce inflammation
Through a full health consult and/or additional functional test i.e. D.UT.C.H. test, your naturopath will know the best course of action for your hormonal type, to support your journey correctly.
FOLLOW US AT: | ||
|---|---|---|
REFERENCES |
|---|
Lara Briden, Period Repair Manual (2nd Ed).
Prior JC. Progesterone for Symptomatic Perimenopause Treatment – Progesterone politics, physiology and potential for perimenopause. Facts Views Vis Obygn. 2011;3(2): 109-20. PubMed PMID: 24753856
https://www.yourhormones.info/hormones/progesterone/
https://www.britannica.com/science/corpus-luteum
DUTCH Treatment Guide – https://dutchtest.com/supplement-guides/
Altman D, Falconer, C, Cnattingius S, Granath F. Pelvic organ prolapse surgery following hysterectomy on benign indications. Am J Obstet Gynecol. 2008 May; 198(5):572.e1-6. PubMed PMID: 18355787
Komorowska B. Autoimmune premature ovarian failure. Prz Menopauzalny, 2016 Dec;15(4):210-214. PubMed PMID: 28250725
https://my.clevelandclinic.org/health/diagnostics/22681-anti-mullerian-hormone-test